|
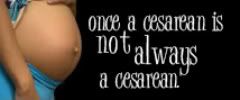
| Photo credit: An Empowered Birth FaceBook fan page. |
I love this photo. Interestingly enough, I wrote my blog post before placing it and realized pretty much everything I said echoed the sentiments in this photo.
If you were a marathon runner, would you try to run the Boston Marathon after only training for a week? A day? Probably not.
Preparing for birth can be like running a marathon - although to some women, "preparing" means different things to different people. It seems that few realize the mental and physical preparation that should go into preparing for birth.
When I look back on what I knew (or, rather,
didn't know) before having my children, it honestly kind of scares me. I distinctly remember my first due date approaching, the baby was breech, and I was excited to meet my child. The doctor told me that if I showed up in labor (a very real concern of mine) they "wouldn't let me go too long" before sectioning me. That was about the sum total of his counsel when it came to the risks and benefits of surgical birth. I scurried (or waddled, probably) to my car in the parking lot, anxious about the impending arrival of my new bundle of joy.
I'm fairly certain that had I really known the risks of cesarean birth, I would have rightly been scared out of my wits. I'm also sure that the reason I wasn't worried about that aspect at all was because my doctor didn't mention jack crap about it. Any of it!
This is one inherent problem in obstetrics today, it seems: a sometimes
complete lack of adequate, informed consent. How can we prepare ourselves for that birth marathon when we don't know what to prepare for? There has to be more to it than breathing through some contractions, grimacing through the pain while they place an epidural, and pushing out a baby. I have heard so many women, on the eve of their inductions, say in a panicked voice, "I'm being induced tomorrow and I have no idea what to expect!" Really??
When I think back on my experiences and how they've played out over three pregnancies, there is one central idea that pops out at me: essentially, you have to start planning future pregnancies before the first one is even finished.
It sounds ridiculous, and can be virtually impossible for many women, but that's about what it all boils down to.
Before your first pregnancy is even over, ideally you should ask yourself:
• What are the risks and benefits of cesarean?
How will it effect any future pregnancies and births? (This is key!)
Depending on how good or bad that experience turns out, it can not only influence how you give birth to future children, but can negatively impact your ideas on how future births may play out (which may or may not even be realized) - and some may decide to scrap their plans for a larger family and opt never to become pregnant again!
• What is my doctor's cesarean rate? More importantly, what is his/her induction rate? (Studies have shown that in first-time mothers, induction can dramatically increase the risk of cesarean section.)
• How can I avoid an induction or cesarean?
• How can I prepare myself for one if one or both become necessary? And how does my doctor define "necessary?"
Another thing that stands out to me throughout my experiences and in hearing others talk about theirs, is the idea that everything our doctors do to us and for us while pregnant and laboring is always for our benefit, and therefore always necessary. This is where you cross into a gray area, I think: some inductions and cesareans are unavoidable and quite necessary, while others are sketchy. It can be quite a conundrum.
• What if I need to be induced for having a 'big baby?' What *is* a "big" baby? I think you'll find a wide range of answers.
• What if my fluid level is low? How can I increase fluid levels? Is it really always cause for alarm?
• If I need to have a cesarean, can I request one that is more "mother-friendly?" This may entail delayed cord clamping, immediate skin-to-skin contact and immediate breastfeeding. If your doctor refuses to do this, ask why - challenge the answers if they seem hesitant or cannot give you any compelling reasons why you couldn't do this (barring an emergency or "crash" section, obviously).
Another unfortunate problem is the "bait and switch," where doctors appear to be supportive of your concerns and ideas but then mysteriously change their minds at the end of your pregnancy. This especially happens with VBACs, where a care giver seems to support the mother's wishes and then poof! Two weeks before your due date they're pressuring you to schedule a cesarean. It sounds paranoid and terrible, but all I can say is, be prepared. If your doctor is threatening you this way, know your rights, know the risks and stand up for yourself the best way you can. Hire a doula, if possible.
Something else I've noticed in talking with pregnant women and in the general population at large is that if it didn't happen to them, then it probably doesn't happen. *eyeroll* Birth trauma is an especially touchy subject for many to discuss, because so many people have come to accept these practices without question, not knowing any other way. One set of health care practitioners will be bold enough to assume that just because no doctor they've ever worked with does inductions without just cause, surely they all operate like that - while another group can vouch that many are truly "cut happy" and have a reputation for rushing through things. This tends to silence women who stand up to the bullying tactics of some care providers, marginalizing their experiences and making others think they're "conspiracy theorists" because they dare to care or push for something better for pregnant women.
If I could do it all over again, ideally I would've been more prepared with that first baby - asking more questions, demanding answers, and informing myself more. My suggestions to you are:
• First ask yourself what kind of birth you want. If you want an epidural and all that jazz, fine, have one! But be
adequately informed of their benefits as well as potential risks and side effects. You have to have more of a knowledge of them than "they're safe, get one!" because that is garbage. If you're on the fence, research your options and know that there's more out there than just that. Keep an open mind about those options and how you can cope without them, including water birth, massage, walking, standing in the shower, etc. But certainly don't feel like a failure because you "caved" and asked for the epidural.
• Take a good childbirth class. This can be subject to personal opinion, honestly. To me, a "good" childbirth class entails informing you adequately about a number of options while not making you feel demonized for choosing an alternative. For instance, if you know you want a natural birth but your teacher is making you feel like an idiot for choosing one (especially issuing the ubiquitious phrase "You won't get a medal for doing it without drugs!") then perhaps that class isn't "good." Likewise, no childbirth educator should make you feel like crap because you want an epidural, nor should they gloss over the risks of them
or make them sound like the Devil's poison, either.
• Read. There is a lot of material out there, (some really good and some really, really bad) and good material will back itself up with
sources. However, I suggest getting your information from a lot of sources, not just one (that includes your doctor). Again, it all depends on what you want in a birth, but some sites will sway in one particular direction or another. An even mix is key: anyone that makes you feel bad for going off your diet occasionally or like everything in pregnancy is to be feared and avoided might be over-the-top. And likewise, someone that acts like there is only one way of doing things, ever! might not be an unbiased, objective source of information, either.
• Avoid people who cannot or will not give you encouragement. This is especially important if you are attempting something that most people consider unusual, risky or not "mainstream" (eyeroll) like home birth, VBAC or really, a completely unmedicated childbirth. More people than not are going to gasp, their mouths dragging the ground, and look at you like you have spontaneously grown four heads. While some people are just uninformed but well-meaning, it's probably best to steer clear of people who can't support you in your efforts and do nothing but tear you down (that includes care providers, too!).
• Realize that when it comes to labor pain, it's all subjective. If you haven't gone through it before, it's normal to be scared about it - but you never know how
you are going to handle it. When people relate their horror stories to you, you have to realize that that's their interpretation of it, not necessarily how it's going to work out for you. There are so many ways you can manage and cope with it without having to immediately ask for drugs - although there should be no shame in that, either. Just realize one thing: that some hospitals make it intentionally difficult to use these coping strategies effectively, such as "not allowing" you to get into a different laboring/pushing position, insisting on continuous fetal monitoring (that can confine you to bed), among other things. Ask about a tub. Ask to move around. Don't be afraid to
just ask and focus on your labor, not pleasing the staff or trying to be "nice" just for them.
• In the end, realize that sometimes the things you desire least may be unavoidable. Being emotionally prepared for this, while not dwelling too much on the negatives and "what ifs," as well as being involved in the process and made to feel like you are an active participant, rather than just a helpless bystander, can help tremendously when it comes to accepting those outcomes. When it comes to being empowered and informed, it may not prevent every intervention, but it sure can't hurt.