Perhaps the finger of guilt is being pointed in the wrong direction. It's not really the consumer who is defrauding the insurance carrier; in the case of a typical hospital birth, maybe it's the physician.
The standard of care in obstetrics is to perform the same excessive battery of tests, monitors and other expensive interventions - that normally would be performed only on a high-risk patient - on every pregnant woman, often whether they need it or not. Suddenly everyone is high-risk. And I'm sure those interventions come with a hefty price tag.
And correct me if I'm wrong, but don't some OB's balk at attending Medicaid-covered patients because a government payor is less likely to pay for certain procedures than a traditional insurance carrier? Wait a minute ... maybe I do want the government running my pregnancy healthcare after all...
I switched OB's for my third pregnancy, and typically under my health plan, all prenatal visits are covered. On three separate occasions, I was billed a copay: once during my first visit (I don't remember ever having to do this with the old guy) and again when my doctor and I had a "conversation" about a VBAC - which basically consisted of her lecturing me in a nice way and feeding me inaccurate information. I considered this part of my pregnancy care and planning, together, the birth of my child; she considered it a consultation.
The third time, they noticed some swelling in my lower extremities and that my blood pressure was elevated. Nothing new from my last pregnancy (and I wasn't billed for it then, either), and apparently not that uncommon in the rest of the pregnant population. But no - this was considered "outside of the scope of prenatal care" and I was again billed. (But apparently that brief hospitalization for observation was considered part of regular prenatal care, because I never saw a bill for that one. I mean, isn't everyone admitted briefly for observation during their pregnancy??)
After awhile I was beginning to wonder if my doctor was nickel and diming me to death just to eke out as much money from me as he could in addition to what the insurance company was paying out. I realized later that, because they were so overbooked, she had charged me a copay because I had questions. And actually wanted answers. Which was much more than I got from the other guy (Me: "I wondered about why I never had the urge to push during my last labor." Him: "Oh, don't worry about that. We'll help you with that when the time comes."). If he talked any more to me, he'd have to charge me for it. Because, when you're herding a dozen or more pregnant women through the door every day, time is money, you know!
I can't imagine if I had been completely new to pregnancy and birth, with no information whatsoever, trusting my doctors implicitly and feeling like I had no need to question them. They basically have no time to tell you anything of consequence except weigh you, collect your pee, measure your belly and dismiss you.
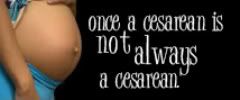
Fast forward to the birth: again, no time to wait on things like slow labors, broken waters with no sign of labor in sight (one site, albeit an article published in 1999, suggested inducing if labor hadn't started within four hours), or first time mothers who are slow to dilate. You get the idea. The clock is ticking! As a result, the inevitable unnecessary induction is scheduled, often leading to the ubiquitous unnecesarean.
Enter insurance fraud.
Personally, I think doctors with high rates of induction and c-section should be investigated. Unless you're a high-risk doctor (and really, everyone is now, no doubt, because isn't pregnancy a risk?) there is no reason why doctors like the one mentioned on the Birth Sense blog (Aka "Jack the Ripper," God help us!) should get away with such abuse of their power and the tools to carry it out. Do you ever wonder if someone who is processing the claims these doctors submit thinks, "Wow, Dr. So and So induced nearly a dozen patients in X amount of time," or "Dr. So and So sure does a lot of c-sections."
We know that a c-section costs more to do than a traditional vaginal birth, as it should. But consider this: when you tally up the cost of anesthesia, the supplies, this that and the other that are all part of a claim, it is expensive. Multiply that by the number of women having c-sections these days (around 32 percent), and you have a booming "industry."
And since a vaginal birth tends to be cheaper, there are easy ways to quickly run up the tally: IV fluids. Induction of Pitocin, several doses. Epidural or similar anesthesia, several doses. Introduce complications such as shoulder dystocia or fetal distress, use of monitoring (which is pretty much done to everyone, regardless), drugs to revive or resuscitate the baby, etc. and that's more money that's ultimately tacked on to the bill. Some of it's warranted - saving your baby after a uterine rupture during a, let's say, non-induced VBAC, for instance. (i.e. something that inherently could not be helped and was not caused by either a medical error or unnecessary intervention)
Not to mention that in the case of a complicated vaginal delivery or c-section, you will probably require more monitoring from nursing staff, as will your baby, and usually a longer hospital stay. Perhaps even minor surgery to repair damage caused by such a traumatic, rushed birth. Multiply that "cascade of interventions" by the number of women who are induced - sometimes for real reasons, sometimes not - in this country, and again, you have a booming business. CaChing!
Not long ago The Unnecesarean posted about billing costs in pregnancy and delivery. Many readers who commented through the FaceBook link remarked how their c-section births were upwards of $45,000. (Yes, that's thousand.) Still others said they or their insurance companies were getting billed for procedures that never happened in their births:
After my DD was born, I received the actual itemized list of charges that the hospital submitted to my insurance company. I was at the hospital about two hours before she was born and left 23 hours later. The only intervention I had was a heplock. I was charged for pitocin I did not receive and I was charged for anesthesia I did not receive. I called my insurance company about this, and they just shrugged it off.If this isn't insurance fraud, I don't know what is. And even more alarming is that her insurance company couldn't have cared less that she was attempting to save them several thousand dollars.
If more OBs were penalized for excessive interventions and surgeries that weren't warranted, perhaps it could open some eyes in this country about the abuses going on in maternal care. (Unfortunately, I realize the lines are blurred in what's considered truly 'necessary' and what isn't.) In a perfect world, it might help, in some way, to lower the c-section rate because now the people responsible for paying the bill are starting to pick up on how much over-billing is occurring. (I'm convinced that if it were any other division of medicine, this investigation probably would have already happened by now.) They've already been talking of 'de-incentivizing' certain maternity costs that mean the OB would get paid the same, regardless. While this might stop some abuse, I'm not sure how well it's working, and do think that surgery should cost more because of the level of skill involved. But it certainly shouldn't be used to the point that it is.