 |
| Photo credit: Brian Hoskins |
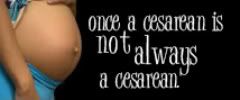
I reposted this article on FaceBook yesterday and have been thinking about it ever since. The use of the word "need" irritates most people, including me. But there were some other things that set me off.
It underscores, among other things, the absolute garbage medical practices that pervade in obstetrics that not only put mom at unnecessary risk, but her baby as well. What Nurse Jenna's article does is unintentionally admit that often the best interests of both mom and baby are not in the forefront. In the very opening paragraph of her article, she sets a rather condescending tone:
Many women come to labor and delivery fearing Pitocin, loathing Pitocin, and swearing up and down that “over their dead body” will they have Pitocin to augment their labor.Truth be told, if anyone knows how miserable Pitocin can be, they've probably heard it from other women who have been there, done that. This winter my niece was facing a (basically unnecessary) induction and everyone on her FaceBook were telling her to "avoid the Pit! It's miserable! You'll hate it! Don't do it!" You would have thought she was contemplating suicide, their tone was so adamant. Did she listen? Nope. (Because, after all, we were a bunch of "uneducated women" and her doctor "knew best.") She ended up getting induced and having a horrible labor, although I still haven't heard the details and am not sure I really want to.
Nurse Jenna sort of tries to absolve the doctors and nurses of their guilt over improperly administering Pit by taking the "blame the mother" approach: moms don't stay home long enough, want pain medication in early labor, and in the comments section, moms "insist" on being admitted before they're actively laboring. No where does she really say that doctors are doing it all wrong, but rather, "We want the mother to stay home as long as possible." She mentions how "we" want you to labor comfortably at home in the early stages, where you have access to food and fluids, supportive family members, a bathtub, etc. Seriously?! (Because we all know that once you enter the hospital, all of those things are often restricted to you, even though they can help progress your labor tremendously.)
While I agree that staying home until you no longer feel comfortable is the best idea, a) this seems to contradict what hospital staff often tell us and b) it doesn't necessarily mean you won't be given Pitocin, regardless of whether you need it or not. According to Dr. Roberto Caldreyo-Barcia, former president of the International Federation of Obstetricians and Gynecologists, "Pitocin is the most abused drug in the world today."
Because there is such widespread misuse and abuse, patients often think it's totally normal. Few are going to tell you "Hey, you don't really need this stuff, you know. You can refuse," and instead make you feel like the bad guy if you don't do it. Your baby is the weapon of choice against you, and a powerful one at that. Nurse Jenna's article also highlights how trusting some are of the medical profession and just put everything in the doctor's hands. Many mothers, especially first-timers with no prior experience, will take their doctor's advice as the gospel and comply, even if it goes against their better judgment or wishes. They don't want to be seen as difficult, and if you appear to be questioning your doctor's judgment it could be a long haul for you as the patient. Of course she doesn't mention fetal distress, the rising rate of cesareans and how induction can contribute to that, especially in first-time mothers. And the idea that, even in a woman who is laboring well on her own, maybe with an irregular pattern of contractions (or not even) you might still stand a good chance of getting it. I wonder if this is less about freeing up beds and more about "Ok, let's get it over with so we can move on to something else."
(Case in point: my neighbor had her second child in May, this time going into labor on her own. Labor had slowed down, apparently, and her well-meaning mother-in-law told me that she was given Pit and "the baby was born 20 minutes later." What?!)
Nurse Jenna's post illustrates the problem our maternity industry has in general: more beds are needed, so let's rush things along over here to make room over there. That is not good medicine, and treats the patient like a number or as if they're giving birth on an assembly line. (Which explains why some maternity units are unaffectionately called "baby factories.") How many women do not even get to this point because their due date falls near a holiday, someone's vacation or other important event? People have criticized the idea that "OB's golf, so they need to induce you so they can be there for tee off." Maybe not golf, but the idea that they do not want to be "waiting around all day/all night for you to deliver" is pervasive, so don't kid yourself. The days of your OB rushing in at 11:30 at night in a tux (like my mom's OB did in delivering me) are long over.
While Nurse Jenna blames mothers on "insisting" they be admitted early, I wonder how common this is. It seems more commonplace to keep mothers who should be sent away because you'll simply Pit them into oblivion. I've also read accounts where they aren't "allowed" to go home, even though they want to. Staying home longer is probably key in reducing your risk of getting Pit, but how many of us have heard, "Well, you don't want to deliver in the backseat of your car/on the toilet/in a public place, now do you?" Many women who are in the advanced stages of dilation but not in active labor are sent directly over to the L&D unit ("Do not pass go, do not collect $200!") to be induced when they don't even want to be, including a woman commenting on Nurse Jenna's post. Just because you're 4 cm doesn't mean "it's time," and even though it's not what mom wants, she somehow feels compelled to cave, often because of pressure from her physician.
I'm sure doctors and nurses grow increasingly frustrated at patients who know little and "insist" on care they think they should be receiving, when really, there is an alternative. Instead of accusing, though, healthcare providers should be informing, and telling patients why you should go home - but I think that would reveal other faults on behalf of the hospital and they're not willing to admit to unnecessarily aggressive induction practices. Conversely, it seems that if you know too much - enough to question and refuse - you're treated like crap then, too.
More women probably stay because they don't realize they have a choice, rather than because they "insist." In my time both as a hospital employee and a patient in L&D, I have never witnessed a mother becoming belligerent because she can't stay. And never, in all my talks with mothers, have I heard someone say "I insisted on staying in the hospital because they were threatening to send me home!" Usually, mom thinks there's something going on, hospital staff say no, and she's sent home, tail between her legs. (Yet all the while with the threat of "You don't want to give birth in the car!" hovering in the back of her mind, right?)
Basically, Nurse Jenna is part of the greater conundrum of "modern" obstetrics: don't stay home too long, don't get here too early. If you want to walk, stay home (one L&D nurse's comment). If you walk while in the hospital, it means you can't be hooked up to monitors and machines, but it could progress your labor - but still, don't walk. If you get here too early, going home is not an option anymore. If you labor at home, you'll be punished for not seeking medical 'care.' If you come to the hospital too early, you'll be punished for seeking medical 'care.' So deal with it. Either way, you can do nothing right and it's your fault.
Some of the comments on Nurse Jenna's article are interesting, and very telling:
The pitocin seriously made me want to kill myself, even after having the epidural. It truly was awful.Unfortunately this woman had come in for induction because her baby had died. After 30 hours of hell, she ended up with a cesarean. (!?)
A failed induction, but hey, thank God for the Pitocin!
i had come in for an induction and had pitocin to get things moving faster the next morning...i didnt care, im not that anal about stuff like that! i know there were other women that needed a bed too! and i am grateful for the pitocin post-delivery/csection to help my uterus contract..At 4 cm but not in labor yet? Who cares! Let's just induce!
I got to the hospital at 4cm, but would have much rather still been at home. I had a severe headache, and dizzyness, and called the dr's office and they sent me in to have my blood pressure checked. I wish they would have let me go back home since my blood pressure was fine (I only live 5 mins away), but instead once they checked me and I was a 4, they called the dr., and he decided to just come break my water. I was so frustrated, because he broke my water and started pitocin and the contractions practically stopped for about 3 hours. But I could get up or anything since they'd already broken my water. I was so irritated because it was not my choice to go to the hospital yet.One commenter kind of blows Nurse Jenna's argument out of the water, and probably many of us can agree:
I certainly was told about "Pitocin-passing" by a nurse. I was in a car accident when I was 24 weeks pregnant and moving to a new city. While they monitored my contractions in the hospital I had a great chat with a nurse who gave me the low down. When I told her I wanted a completely drug free birth she told me which hospital to avoid (named the baby machine hospital because they do so many births and regulate with Pitocin) and which drs. would be sympathetic to a drug free delivery.And probably the best comment EVER:
Who is we? The God's of the delivery room? NATURE decides when the baby will come! I'm glad I was informed and confident in my birth not to let a dumbass like you [be] in control!




7 comments:
I was told if I didn't get Pitocin that I would need a C-section (something I told the nurse early on I was desperate to avoid) or my baby WOULD DIE. Of course I got the pitocin then. I have to say I managed to ride it out without an epidural or too many other interventions though. The only other things that happened that pissed me off were that his cord was cut on delivery and he was taken to the warming table instead of being put on me. I cried for 20 minutes while they "worked on him" even though he was fine. All I could say was "Give me my baby... I want to see my baby!"
I wish I could remember where I read this - mama was pretty dilated at the doctor's office and the doctor insisted she go to L&D. She didn't want to, and the doctor basically said "A police escort will be waiting for you." Lying, probably - but that doesn't exactly sound like the "we want you to labor at home in the tub!" message that Nurse Jenna is advocating.
I saw it in the comments here (the police escort part) http://myobsaidwhat.com/2011/06/24/i-would-force-you-weve-done-it-before/
Yes, that sounds about right, Melissa. Thanks for the link.
I was pretty educated prior to giving birth but when my water broke and the doctor on duty told me I would be on pitocin, I figured I had no choice and that this was routine when your water breaks. I was lucky however, because the doctor who admitted me made me walk the halls to get my contractions moving so that I would be put on the lowest dose of pit which is what happened and I gave birth "naturally" 16 hours later.
One more thing: This taught me that next time, I will be letting them know that I have a choice in whether I get pitocin.
I was so prepared to have a drug-free birth. I researched natural birth for about two years and took Hypnobabies to prepare myself. I saw midwives and went to a birth center. We did very few tests or ultrasounds and I had a perfect pregnancy. But after about 70 hours of labor and being stuck at a 6-7 for 14 hours, I knew I needed help (my water had also been broken for quite some time).
We changed our plan and went to the most natural friendly hospital in our city. I chose to have an epidural to see if it could help me rest and relax but I didn't dilate any further at all...so, I chose to use pitocin. The birth of my daughter was still amazing and a very wonderful experience, despite my "need" for medication. I wish it would've been different, but I truly believe we had the birth we needed for the situation we found ourselves in.
I guess my point is, sometimes there IS a need, but I think it's rare. Unfortunately, I was one of those rare cases.
Post a Comment