|
| What is normal birth, anyway? |
Whenever I have conversations about birth with people and see comments on pregnancy forums, I'm saddened at how our definition of "normal" has totally been taken off course. I don't know why I'm surprised by this, but am continually amazed at some of the lies, misinformation and half-truths that lurk out there, and how the Reality of Childbirth is one big rumor that just won't let itself be put to rest.
When people think of the "history of childbirth," they probably think that there isn't any: how can one woman getting pregnant and delivering a baby be any different than it was 100, or even 1,000 years ago? How can there be a 'history' to a basic biological function that has taken place in millions, even billions, of women since the dawn of man?
I've decided to compile a few of the things that I consider "BS" when it comes to obstetrical practices, starting with our perceptions of what "normal" birth is. Much of it is rooted deeply in myth, some in fact that has been extrapolated (I love that word!) to include everyone now, even though they often present no symptoms and fit no risk categories. We fail to see ourselves as "birth consumers" and trust our doctors to tell us what we need to know, which in some ways we should. But because we often don't understand the mechanics of birth and how it relates to the capabilities of the human body, or the politics surrounding it, we often trust them in ways that we shouldn't. I suppose it's different for everyone, but I cringe whenever I hear people refer to a vaginal birth as
"natural," especially when it's far from it. Natural in the sense that that's the preferred mode of delivery for humans. But that's about where it leaves off. Perhaps they should use the word "normal," but even that's a matter of debate.
If you're like most American women, you get pregnant, find an OB, and think that's the end of it. When it comes to delivery, you know that one of several things usually happen: you are either induced for a variety of reasons, or "allowed" to go into labor on your own time. Occasionally you are "permitted" to go overdue, but not without some level of concern first. You've heard that the placenta can deteriorate after a period of time once the baby reaches a certain gestational age, and it has you worried that you might go
overdue .
You've long-since chosen your care provider. In your case, you probably have chosen an OB, because that is usually just the 'thing to do' when you're pregnant. You've heard a lot about
midwives , but it just doesn't sound like a good idea to you. After all, what if there was an emergency? Your second cousin had a midwife and it worked out for her, but a neighbor told you that
midwives don't know what they're doing and
can't be trusted . You figure that's probably true, because so many people see an OB. Besides, your OB's practice doesn't allow midwives, and neither does your hospital. It's probably for the best.
As your due date looms large along with your waistline, friends start asking:
"When is your doctor going to induce you?" One friend says she was induced at 38 weeks and two years later, doesn't know why, which leaves you scratching your head. Most of your friends agree that your
doctor will only induce you if it's deemed
medically necessary , or if
you're tired of being pregnant or relatives will be in town . A few other friends say how they were induced and in all but one, had
cesareans . "But that's just how it is," says one friend, shrugging her shoulders. "No big deal." You know that one friend was induced because of a baby they thought would be
big , weighing a little over 8 pounds. You worry, but don't think too much about it and remain happily pregnant a little while longer, but you are concerned that something might be wrong when your doctor brings up induction at every appointment from 36 weeks on. You ask him about it and he shrugs you off like it's no big deal and says, "See you in two weeks!"
If you haven't been induced by now, you're probably laboring on your own. The next course of action is often to administer Pitocin, sometimes even if you have a
regular pattern of contractions . This is often just to speed things up, even though you're doing fine. Assuming that both you and the baby's heart rate look good - detected through external continuous fetal monitoring, of course - you will be "allowed" to continue laboring, usually. If it takes a
long time , though (and everyone's definition of "long" varies), other things might be considered, usually resulting in more Pitocin or eventually a cesarean.
If you haven't been sectioned by now, you might be experiencing stronger, more painful contractions. Your doctor might tell you "No, that's not any different than normal contractions," and if this is your first baby, you have nothing to compare it to, so you don't question it. You request the epidural, and you can't get up and move around now that you've been confined to bed. Your hospital dictates that you
can't have fluids and food in labor , so you're near exhausted and just want this baby
out. However, the epidural is administered - either it doesn't take and they have to give you another one, or you muddle through without it - flat on your back, in agony. The baby is starting to go into
distress , which worries you. The doctor looks concerned and tells you it's time to consider a cesarean. At no point has anyone suggested
turning down the Pitocin .
Finally it looks like
progress is being made. At first you are worried because the doctor says you're
"not progressing fast enough," even though you are a first-time mother who has only been laboring for less than 10 hours. You've been pushing for what seems like forever, even though you have
no urge whatsoever. You're seeing stars and getting light-headed from holding your breath and
pushing when they tell you to , and it's so hard to push the baby out that the doctor begins to use vacuum extraction. You feel intense pressure and tearing that feels like your insides are being ripped out. And then, the baby is born and it's all over. Thank God!
You hold your baby for a brief moment and then she's
whisked away to a warmer. They don't want her to get cold, and after all, there are those very
important tests to perform to make sure she's okay. You want to hold your baby, but you know all those tests and everything are necessary, so you watch as nurses huddle around her in the isolette and
swaddle and bathe her.
Then you're taken to your room and the baby is finally handed to you a little while later. You try to nurse, but it's kind of difficult because you're a first-time mother, after all. She's not very interested in breastfeeding, likely because you had several doses of the epidural after the first one didn't take. Finally she latches on, but a nurse tells you that
you can't do it and your nipples will start bleeding and get excoriated and
it hurts too much . What she doesn't tell you is that they've already given her a bottle of formula without asking because your
baby's blood sugars were low , and you don't realize she has nipple confusion. The nurse is breathing down your neck, the baby is crying, and there is a huge bag of formula
"just in case" you needed it. You decide to use it because the
baby seems really hungry , or at least the nurse thinks so.
The doctor comes in and tells you you did a "good job," and that it might be advisable to have a
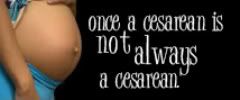
planned cesarean the next time, just in case . You agree, because, after all, he's the doctor and knows what he's talking about.
Fast forward six months. You've had time to heal, you love your baby, and she is thriving. You're at a baby shower for a friend, surround by aunts, your sisters, female cousins, and coworkers. You're sharing stories with each other about birth - and they ask you, since you're the last one to have a baby - how it was. You tell them, frankly, that it was the worst thing in your life, terribly painful, but so worth it for this wonderful daughter you have. Based on your story, most of the room agree that when they have children, they are "definitely getting an epidural!" One says, "My mom had c-sections with me and my brother, I'll probably have to have one, too." Another says, "Yeah, my grandmother had a vaginal birth with my uncle and she nearly died!" Still another says, "I had a natural delivery. They had to give me Pitocin and do an episiotomy, but all I had was Demerol while in labor. It wasn't too bad."
The seed of doubt has been planted. When everyone you know has had the same "normal" experience, not realizing that it's anything but, it suddenly takes on a life of its own. The idea that our bodies are somehow defective has taken hold and runs rampant, like a bad rumor that just won't die and go away.
And so is our definition of "normal" childbirth.
More reading:
Tabby Biddle: Women Speak Out About What's Gone Wrong with the United States Birthing System
Melissa Bartick: Peaceful Revolution: Motherhood and the $13 Billion Guilt