The blogger at Birth Without Fear has been writing some wonderful, heartfelt posts lately about the upcoming birth of her fifth child, which she is planning to do unassisted, like her last. While I have never had an unassisted pregnancy or birth, I can relate to what she is saying on so many levels, and I find her writing to be quite wonderful.
She has recently written about her desire to have an ultrasound, even though she is presumably doing the rest of the pregnancy, and hopefully the birth, unassisted. She confides in us that she has been having unexplained fears and some thoughts about the baby and upcoming birth and feels that she needs to have an ultrasound to make sure everything is okay. While I don't know ultimately whether she will get one or not, or already has, she has been getting some flak from some in the birthing community - that perhaps say she isn't trusting enough in the birth process or in the ability of her own body to birth a baby. Part of the criticism, I think, is because she's considering relying on technology that is considered, to some people, to be wrong, dangerous, or unnecessary.
I find this kind of sad. As I said on her FaceBook page, I think sometimes other birth advocates can be a tremendous source of support to each other, and at times we're our own worst enemy . To some, BWF's decision to birth at home unassisted is foolish; to others, it's brave; and to still others, it's the only way to go.
I can't say I'd ever intentionally do an unassisted birth, and yet I have day dreams about setting up the back of my husband's 1996 Safari van as a little haven just in case I should happen to give birth while en route to the hospital. I picture the baby coming out perfectly, and bringing him or her to my chest - no separation, no interference, just me and my husband. I can see, especially given the traumatic births some women have experienced, why they would choose home or even unassisted birth. I imagine that takes an amazing level of faith in oneself and calm that some people cannot understand.
For me personally, my birth faith is not so much derived from myself, but from my belief in God. I've always wanted to write a post about the spiritual aspects of giving birth, and was never sure how it would be received. I realize not everyone shares the beliefs I do, and I'm not even sure some Christian mothers experience the feelings that I did. In my experience, I know the intuitions and feelings that BWF is experiencing, and some are no doubt just plain old normal fears that come with being a mother, and some might be founded. While some people think the idea of God speaking to them is crap, I don't: I know that many of the intuitions and feelings I had while pregnant and in labor were that still, small voice in my head telling me, 'Do this, don't do this.' Somehow, it all worked out for greater good and events fit together like puzzle pieces.
While in labor with my VBAC baby, I stayed at home as long as I felt comfortable. Something told me to eat before leaving the hospital - I had been up since early morning and had not felt like eating. I was beginning to feel nauseated and emotional for no reason, and in hindsight, this may have been the beginning of transition. I ate two pieces of buttered bread and a small glass of orange juice and was on my way to the hospital. Before getting there, though, something made me want to stop at the grocery store to stock up on magazines and water for my labor/hospital bag, and I paced and walked through contractions. Something told me to keep moving and remain upright. When I got to the hospital, I was about 6 cm (pretty good for my first vaginal birth!) and delivered about three hours later.
While pregnant with that child, it was a tremendous leap of faith, some would say, just to reach the point to decide to have a VBAC in the first place. There was nothing saying that, even with no interventions, that I wouldn't have another cesarean or that something catastrophic wouldn't happen. I prepared myself physically and emotionally, as well as spiritually: I prayed every chance I got, while walking, while rocking, while sitting on the toilet, even. I prayed that God the Divine Physician would give me confidence and strength to know when to make certain decisions, and that he would guide me through labor. I prayed that he would put his hand over my scar and protect me. And he did.
When I was pregnant with my third, I was again planning a VBAC. At one point during my pregnancy, I sat quietly - probably on the computer! - and a clear voice in my head told me, "This child is a boy and will be born by cesarean." I had no reason to believe either - we had not found out the gender and the baby was head down, so things were looking good for a vaginal birth - and I kind of frowned to myself and forgot about it. As I approached my due date, I was having trouble with elevated blood pressure and rather unsupportive OB's, and - surprise! - my baby had turned transverse and later breech. Even after being admitted for observation and refusing a cesarean then, I trusted my body - and God - to tell me when it was time and when it was not, and to guide me to make the best decisions for my baby and myself. I decided to go home and rest, wait to see if the baby would turn, and let him or her pick the day to be born. I also prayed I had a quick, painless labor and an easy vaginal delivery.
As the day approached, those intuitions kicked up again. The night before, something told me, "Don't finish all your dinner." I was kind of hungry, but had no desire to eat. I left most of my plate untouched and tried to rest. By 10 p.m. I went to bed but was having mild contractions that kept me awake much of the night. I do know I managed to sleep and even dream, but by 4 a.m. I was now in full-blown labor and had lost my mucus plug. Not knowing what position the baby was in, I packed up my stuff, ate my usual bread with butter and orange juice, and left for the hospital.
By the time we got there about 35 minutes later, I was fully dilated. My water had narrowly missed breaking all over our freshly-detailed interior. When they did an ultrasound to verify the baby's position, the baby was breech. I was more worried about them accidentally revealing the gender right before the birth than the impending cesarean. And while a nurse confided in me that my baby could be born vaginally, I knew in my heart that I was not willing to risk it if my unskilled doctor hadn't delivered a footling breech baby in probably a decade or more, and told her as much.
When they delivered my son by cesarean, I thought back to those words I had heard in my head and knew my intuition had been correct. It was like a warning bell that prepared me for what was to lie ahead, even though I had tried to ignore it. What I knew was that I had trusted God to let me know when to do what, and trusted my body as a machine created by him to do great things. But it is not perfect.
I often think back on how I was perfectly ready to have my baby at home, with just the EMS squad - who I knew have not delivered a baby before. I wonder, how would we have handled the birth?
We are blessed with mother's instinct and intuition for a reason. While I am a strong advocate for natural birth - as much as reasonable or possible - it is important for us as advocates not to be so arrogant or too trusting to assume that things can't go wrong even when there are no interventions present. In the end, you can trust birth all you want, but unfortunately things can go wrong, babies die, sometimes whether their labors have been "tampered with" or not, and some people are unwilling to admit this. Things can happen, but this doesn't necessarily make birth inherently dangerous. But it's a fine line to walk.
You might find that, had you not acted on your suspicions or feelings, something terrible would have happened. You might also find that nothing whatsoever is wrong. And then again, you could be feeling great the entire time and not see for a minute that something is around the corner. Sometimes an intervention can prevent things, sometimes not; but to say that "had you only had a cesarean, your baby would have lived!" is often misleading and wrong. You cannot live your pregnant life in a bubble, hooked up to monitors and machines the entire time to catch such a rare moment, should it happen. You should not be made to feel like you're doing something wrong for judiciously using that same technology, even if it is just to make sure. Nor should there be an approach that suggests "nothing bad will ever happen, because I can do this!"
I don't think birth is dangerous or safe - there is a variable there that can only be measured on an individual basis and we can't always assume that it is or isn't for everyone. We can't always assume that X happened because a doctor did this, nor can we say that nothing bad will happen because you're under a doctor's care, either. Not always can we predict the unpredictable, and if your innermost feelings are telling you something, then perhaps it would be wise to listen.
Related posts:
Home Birth Death: Are Pieces of the Puzzle Missing?
A Journey to Homebirth: Part 2
Where I Stand Now: Birth after Cesarean
Recent Posts
Tuesday, November 30, 2010
Saturday, November 27, 2010
"I want a baby sister!"
Posted by
The Deranged Housewife
 |
| Brothers are wonderful, but there's something about sisters that's magical. |
And I have to admit, that no - I don't "feel done." What a big step it was in finally admitting to myself - saying out loud! - that I wanted another baby. There is no overwhelming urge to quit having children and leave my son's babyhood behind. I am reluctant to cut his hair, despite it growing into his face and making him look like I already do have two daughters, because it is symbolic of his babyhood. I'm still nursing and quite happy about it, and so is he, Boob Man that he is.
When my youngest was probably less than 24 hours old, I had that familiar pull that I wanted Another Baby. I thought to myself at the time, This is ridiculous. Feeling let down or ripped off by an unplanned cesarean is one thing, but wanting another baby? I felt like I only wanted another child because of some kind of "do over," which seemed silly and drastic. Why did I want another baby when this process - going through a lack of support to try another VBAC, high blood pressure and borderline pre-eclampsia, and being "old" while pregnant were hard enough the last time. Ballooning to just over 200 pounds at birth did not help, and that's one thing I do not care to repeat again. I distinctly remember the nurse asking me my weight while in the presence of my husband, and I flatly told her, "I don't know." LOL
I waited patiently for that Baby Urge to go away, and even though I was getting up twice a night with an 18-month-old, struggling with three and doing mountain after mountain of laundry, it never went away. I'd sit at night nursing the babe, exhausted, and think, Maybe I don't want another baby. But I could never quite push it out of my mind.
I thought on it for months and realized how much I absolutely love the image of heavily pregnant mamas, herding their two or three little ducklings around in public. There is something so wonderful about the image of a large family, despite what our modern society thinks about it. I have several step and half siblings, but none from my parents' marriage, and while there are merits to being an only child, I always yearned in some ways for a sibling.
There are those usual concerns - my age, the space between siblings - that people often mention. The other day I was thinking, 34 isn't too old to have a baby, what am I worried about?! Then I remembered, Wait a minute - I was 34 when I had my last baby, I'm 36 now! I distinctly recall being pressured into ordering extensive tests because I was going to deliver a baby at "an advanced age," and I think so many women are scared into not having the children they otherwise would have by an overbearing care provider who has them convinced that their uterus is going to shrivel up and fall out once they hit their 35th birthday. Since I just turned 36, I haven't noticed anything particularly alarming in that area, and as far as I can tell, my parts are all still where they should be.
A lot of people I've talked to express concern over age gaps between kids, which I think can be as much crap as it can be valid. I am 12 years older than my youngest half brother, and while we're not particularly close, being raised in different households didn't help, I'm sure. My three stepsisters are close despite being raised in tumultuous situations surrounding the death of their mother when they were young. I once dated a guy whose parents waited several years after their second baby in hopes that the third child would be closest to them, while the older two would be close to each other. The exact opposite happened - the oldest and youngest were close, while the middle child was - and is still, from what I hear - practically attached at the hip to his parents.
There is nothing saying that they will get along and be all happy giddy, but neither is there anything that says they won't. My oldest two, after all, usually fight like cats and dogs, but they love their baby brother, and he loves them.
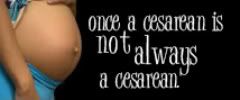
I decided, as time went on, that yes - part of it, a small part - is the hope that I can get a do over. I was particularly encouraged when ACOG restructured their guidelines about VBA2C being safe for some women, even though I know that doesn't mean any doctor in my area will support my wishes. Through my FanPage I've found excellent support and resources from other women and midwives that suggest yes, I can VBAC after two cesareans, which brings me even more hope and encouragement.
Much like while I was pregnant with my third baby, I desperately want to give my daughter a sister. I know there is nothing saying that if I do get pregnant we'll have a girl, but there is that inkling. There is something wonderful about brothers, yes; but something truly magical about sisters. I would love to be able to give her what she's asking for. I know that, if we do have another, that things might not turn out the fluffy fairy tale that I'm dreaming they will, but I'm willing to take that chance.
Wednesday, November 24, 2010
The myth of the emergency c-section
Posted by
The Deranged Housewife
It seems like when you're talking about a c-section, it often comes down to a question of semantics. The word "emergency" gets thrown around an awful lot, and I can't help but wonder if there's any validity anymore to the "If I didn't have a cesarean, my baby and I would have died!" argument.
Nowadays it seems that everyone has had an "emergency" cesarean. Come to think of it, depending on who you ask, I've had two of them.
To some, it seems like if labor has started and it's obvious a vaginal delivery won't take place, it suddenly becomes an emergency. I read one comment on a birth forum about a woman asking what happens when you go into labor before a scheduled cesarean, and the response - from a labor and delivery nurse, no less - was, "Your scheduled cesarean becomes an emergency cesarean. No big deal." Aren't emergencies usually a big deal? And what about this is indicative of an emergency?
In my situation, I went into labor before a scheduled cesarean. I came to the hospital in plenty of time, and was 4 cm upon arrival. Even if they had left me sitting there for a few hours, I probably would have been just fine. Was this an emergency? Not really.
Even after my second cesarean, when a nervous soon-to-be-new dad asked me if it was an emergency after hearing the hairy details of the birth, I sort of shrugged. "Yeah, I suppose you could say it was emergent," with an air of hesitation. I was already fully dilated when I got there, but had no urge to push and no little feet were sticking out. Emergency? Probably not.
Nothing confirms my suspicions about the true nature of emergency cesareans more than this comment from My OB Said What?!?:
I've heard countless comments like that from so many people and wonder what the real back story was. I wasn't there, obviously, but the minute they mention the words "induction" or "Pitocin," I cringe inside. They don't even realize their "emergency" was likely brought on by the actions of their physician, who either meant well or was deliberately putting them at greater risk for his or her own purposes. Putting on a sympathetic face and frowning while saying "You're going to need an emergency cesarean!" sounds better than, "I need to catch a plane and I need you to push out this baby." (Although some physicians no doubt don't bother to cloak it in concern and just tell it like it is.)
I read one such account from someone commenting on a blog post about a teenager who was in labor, and the doctor was pressuring her to consent to a cesarean. As the physician walked out, this person overheard her say, "Thank God she finally consented. Now I have just enough time to catch my flight." Unfortunately, because of this experience, this young mother will forever have the word "emergency" emblazoned on her mind and think her body failed, and it was the only way. Which is a lie.
It's hard, as a birth advocate, to hear these stories. I think for some, it's a mixture of several things: pride, ignorance or misinformation, and a blind trust in their physician. They do not want to admit that they believed their doctor would tell them everything and that he lied. They do not want to admit that perhaps they made a decision that could have turned out better had they only known more. Or they just had no idea that things could be different. Birth stories are something that are shared between women, even strangers, who otherwise have little if any connection to each other and yet are willing to talk about those intimate moments with a woman they don't even know. And thus not only is the birth of a child talked about, but the birth of a myth is, as well.
One mom I know told me that when she delivered her only child in the 1980s, she was induced. Her baby went into distress and she had a cesarean. Another mom had AROM with her first, which produced cord prolapse and an emergency cesarean. (She was, however, able to VBAC twice after that with the same doctor.) Still another talks about how a friend is going in for an "emergency" cesarean at 37 weeks because the baby is "small" (estimated at five pounds, three ounces by an ultrasound, which can be a pound off, either way). (What baby isn't small with three to five weeks to go?!) This mom tried to birth vaginally after being induced, but her doctor, from the looks of it, rushed her into a cesarean after she was dilated to 8 cm after only two hours with a posterior baby. Now she feels like a failure and that her body is "defective." How can you explain to someone that perhaps your "emergency cesarean" was an "iatrogenic emergency cesarean"? That sounds a bit clunkier and hard to pronounce, and still few are ready to listen when told their doctor might have been the initiator.
I posted these terrific articles recently about a hospital in Minnesota that has a very low c-section rate because they use midwives. They show a mom laboring in a tub, without pain medication, and also talk about midwives repositioning a mom in order to birth her baby vaginally. Yet, based on the comments from some people, they still don't get it. Another article - this time from England - talks about the "myth of too posh to push," and still others don't understand. Most are probably in denial that their doctor, the person they have trusted, could ever do something to hurt them or their babies. Many like to put the onus of elective cesarean on the mother and her choices, and to some extent, we can't discount that. But I can't stand the mentality that no doctor will ever do an unnecessary cesarean in the US, because that's obviously not true. If only we could better discern which ones were true emergencies versus those in which the doctor only said they were, for dramatic effect in encouraging you to make your decision faster (i.e. the "Catch my plane" cesarean mentioned above).
When looking at cesarean rates over the last few decades, they have increased steadily just within the last 20 years, in which time we've still had "modern" obstetrics to save us from ourselves in case of just such an emergency. Considering the rates are continuing to climb, what does that mean? That we're evolving into a species that suddenly can't give birth vaginally? That suddenly birth is much more dangerous than it used to be only two decades ago? I wonder, if people bother to look at the stats, if they even for a moment think about the absurdity of what they're saying. And can we quit blaming the mother for everything - from her "preference" to her weight and stature - and for once look at how her labor and delivery are managed by her doctor?
We use the term "emergency" so casually - paralleling the casual attitudes towards surgical birth in general - and water down its meaning until we don't even know what is normal and what isn't, or how to define a life-threatening situation. These attitudes, myths and misconceptions have totally changed not only our attitudes about what constitutes a real reason to have a cesarean, but clouded our view of birth as a whole.
Nowadays it seems that everyone has had an "emergency" cesarean. Come to think of it, depending on who you ask, I've had two of them.
To some, it seems like if labor has started and it's obvious a vaginal delivery won't take place, it suddenly becomes an emergency. I read one comment on a birth forum about a woman asking what happens when you go into labor before a scheduled cesarean, and the response - from a labor and delivery nurse, no less - was, "Your scheduled cesarean becomes an emergency cesarean. No big deal." Aren't emergencies usually a big deal? And what about this is indicative of an emergency?
In my situation, I went into labor before a scheduled cesarean. I came to the hospital in plenty of time, and was 4 cm upon arrival. Even if they had left me sitting there for a few hours, I probably would have been just fine. Was this an emergency? Not really.
Even after my second cesarean, when a nervous soon-to-be-new dad asked me if it was an emergency after hearing the hairy details of the birth, I sort of shrugged. "Yeah, I suppose you could say it was emergent," with an air of hesitation. I was already fully dilated when I got there, but had no urge to push and no little feet were sticking out. Emergency? Probably not.
Nothing confirms my suspicions about the true nature of emergency cesareans more than this comment from My OB Said What?!?:
“It’s extremely urgent we do the cesarean now before your baby goes into stress and it becomes life-threatening. Let me just deliver the woman across the hall and then we can get things ready.”Seriously? If you have that much time to wait, then it must not be an emergency. If this comment had come from anyone else (assuming that most contributors to MOBSW "get it" and see it for what it really is), I'd probably smile and nod and walk away muttering something. It seems like once you throw the word "emergency" in there, suddenly everything comes to a grinding halt and "your baby would have died had you not had that cesarean!" Are you sure about that?
I've heard countless comments like that from so many people and wonder what the real back story was. I wasn't there, obviously, but the minute they mention the words "induction" or "Pitocin," I cringe inside. They don't even realize their "emergency" was likely brought on by the actions of their physician, who either meant well or was deliberately putting them at greater risk for his or her own purposes. Putting on a sympathetic face and frowning while saying "You're going to need an emergency cesarean!" sounds better than, "I need to catch a plane and I need you to push out this baby." (Although some physicians no doubt don't bother to cloak it in concern and just tell it like it is.)
I read one such account from someone commenting on a blog post about a teenager who was in labor, and the doctor was pressuring her to consent to a cesarean. As the physician walked out, this person overheard her say, "Thank God she finally consented. Now I have just enough time to catch my flight." Unfortunately, because of this experience, this young mother will forever have the word "emergency" emblazoned on her mind and think her body failed, and it was the only way. Which is a lie.
It's hard, as a birth advocate, to hear these stories. I think for some, it's a mixture of several things: pride, ignorance or misinformation, and a blind trust in their physician. They do not want to admit that they believed their doctor would tell them everything and that he lied. They do not want to admit that perhaps they made a decision that could have turned out better had they only known more. Or they just had no idea that things could be different. Birth stories are something that are shared between women, even strangers, who otherwise have little if any connection to each other and yet are willing to talk about those intimate moments with a woman they don't even know. And thus not only is the birth of a child talked about, but the birth of a myth is, as well.
One mom I know told me that when she delivered her only child in the 1980s, she was induced. Her baby went into distress and she had a cesarean. Another mom had AROM with her first, which produced cord prolapse and an emergency cesarean. (She was, however, able to VBAC twice after that with the same doctor.) Still another talks about how a friend is going in for an "emergency" cesarean at 37 weeks because the baby is "small" (estimated at five pounds, three ounces by an ultrasound, which can be a pound off, either way). (What baby isn't small with three to five weeks to go?!) This mom tried to birth vaginally after being induced, but her doctor, from the looks of it, rushed her into a cesarean after she was dilated to 8 cm after only two hours with a posterior baby. Now she feels like a failure and that her body is "defective." How can you explain to someone that perhaps your "emergency cesarean" was an "iatrogenic emergency cesarean"? That sounds a bit clunkier and hard to pronounce, and still few are ready to listen when told their doctor might have been the initiator.
I posted these terrific articles recently about a hospital in Minnesota that has a very low c-section rate because they use midwives. They show a mom laboring in a tub, without pain medication, and also talk about midwives repositioning a mom in order to birth her baby vaginally. Yet, based on the comments from some people, they still don't get it. Another article - this time from England - talks about the "myth of too posh to push," and still others don't understand. Most are probably in denial that their doctor, the person they have trusted, could ever do something to hurt them or their babies. Many like to put the onus of elective cesarean on the mother and her choices, and to some extent, we can't discount that. But I can't stand the mentality that no doctor will ever do an unnecessary cesarean in the US, because that's obviously not true. If only we could better discern which ones were true emergencies versus those in which the doctor only said they were, for dramatic effect in encouraging you to make your decision faster (i.e. the "Catch my plane" cesarean mentioned above).
When looking at cesarean rates over the last few decades, they have increased steadily just within the last 20 years, in which time we've still had "modern" obstetrics to save us from ourselves in case of just such an emergency. Considering the rates are continuing to climb, what does that mean? That we're evolving into a species that suddenly can't give birth vaginally? That suddenly birth is much more dangerous than it used to be only two decades ago? I wonder, if people bother to look at the stats, if they even for a moment think about the absurdity of what they're saying. And can we quit blaming the mother for everything - from her "preference" to her weight and stature - and for once look at how her labor and delivery are managed by her doctor?
We use the term "emergency" so casually - paralleling the casual attitudes towards surgical birth in general - and water down its meaning until we don't even know what is normal and what isn't, or how to define a life-threatening situation. These attitudes, myths and misconceptions have totally changed not only our attitudes about what constitutes a real reason to have a cesarean, but clouded our view of birth as a whole.
Monday, November 22, 2010
Technology and birth: Should a robot perform your cesarean?
Posted by
The Deranged Housewife
I don't think Bill Gates realized he was about to open a huge can of worms when he recently speculated, among other things, that robot technology could be used to perform c-sections. The birth nerd community responded, horrified, and the general consensus among my FaceBook friends was that it would basically dehumanize the birth process even more than it sometimes already is.
I think we can all agree that sometimes, technology in giving birth is a lifesaver. And then there are those gray areas, like electronic fetal monitoring, that have a shady, somewhat dubious past, and yet are used constantly even though they have actually been shown to lead to more cesareans, instead of fewer. In some cases, the very thing that's supposed to detect cases of cerebral palsy actually fails to do so, thus also failing to identify which babies are truly in distress and do need to be delivered immediately. In the other half, it leads to more cases of distress that are questionable , oftentimes producing a newborn who is quite pissed off to be so violently thrust into this new world.
I think, therefore, that we need to be vary of our use of technology, especially in surgical births. Having a robot do your c-section might sound cool to Bill Gates, until it's you lying on the table, already feeling like a slab of meat and having that inanimate object hovering over you. If you are distressed or emotional about the birth ending in a cesarean, the robot cares even less than your physician might. It doesn't care if you're crying, upset, or having birth trauma. It can't hold your hand throughout or ask how you're doing. It can only, with another machine, check your vitals, see that you're doing okay, and proceed as usual, completely disregarding any emotional or psychological aspects that can't be registered with a machine.
When I had my first cesarean, their routine choice of medication administration was a PCA (patient-controlled anesthesia) pump. This requires an IV be inserted and the patient then decides when to inject herself with pain medication. According to nursing guidelines in the hospital where I gave birth, I was allowed no more than 10 doses in a one-hour period.
This might be all fine and good, and I can understand why a PCA pump can be helpful, if used properly: it allows the patient to determine her level of pain, while the nurse can tend to other patients. But shortly after being wheeled into recovery - probably the minute the spinal wore off - I noticed that I was in increasing pain, and the PCA pump didn't seem to be doing anything about it. Off and on throughout the middle of the night, the pump would routinely beep at me - and I knew, from my experience calibrating pumps as a pharmacy tech - that that meant there was a problem. The nurse would come in every so often, adjust something, tut about this and that, and then leave the room. A half hour or so later, she'd come back for a repeat.
After the first full day, I had tried injecting myself and nothing happened - except a horrible burning sensation up the length of my arm, which had been happening since I was in recovery - and the nurse scolded me that I had reached my maximum number of doses for medication per hour and couldn't have anymore. The pump had counted the number of doses, and it told her I had already had enough, and that was that. No doubt everything else looked good, and she didn't bother asking me why I was still in pain, even with that much medication supposedly flowing through my veins.
Finally, after my hand swelled up like a blown-up latex glove, the nurse noticed and quickly remarked how they 'had to get that thing out of there.' I had told them, numerous times, that it wasn't working, and that I felt more pain from injecting myself than anything else, at this point. I repeatedly asked, "Is it supposed to burn when I do this?" after another dose of Demerol. It was only after that that I realized the line had infiltrated at the injection site and the painkillers were leaching into my tissues, which offered little, if any, pain relief. No explanation, no apology - I only managed to figure out later that that's what happened.
I consider this episode a major technology fail. A machine can give you so many doses of something and then tell the nurse, in a nice digital printout, how much you've had, when you're due for another, and so on and so forth. It cannot, however, tell the nurse why you're in pain, or that there might be a problem. Only she can do that. And she can only do that if she listens to you as a patient.
I had tried speaking up and no one really listened. If they had been listening, perhaps they would have pulled the entire thing out from the beginning and tried again. Another technology fail lies in the fact that, with increased technology, nurses are then able to spend more time tending to other patients, and thus take on a greater caseload. Additionally, when someone does need something that only a human can respond to, they often become resentful or irritated when you do speak up and express a need that the machine failed to address. Perhaps this is why some OB's are perceived - whether for right or wrong - as cold and callous, because they expect the machine to do their jobs, to some extent: to give them results so they don't have to. In many situations, technology - as we see in the case of EFM - has replaced human judgment, which is an art form that is dying quickly, it seems, when it comes to birth. As a result, greater technology has helped patients, while at the same time, hurt them - by destroying the nature of the one-on-one patient-caregiver relationship. No robot can take the place of that.
More reading:
Bill Gates and Robot Cesareans - The Unnecesarean
I think we can all agree that sometimes, technology in giving birth is a lifesaver. And then there are those gray areas, like electronic fetal monitoring, that have a shady, somewhat dubious past, and yet are used constantly even though they have actually been shown to lead to more cesareans, instead of fewer. In some cases, the very thing that's supposed to detect cases of cerebral palsy actually fails to do so, thus also failing to identify which babies are truly in distress and do need to be delivered immediately. In the other half, it leads to more cases of distress that are questionable , oftentimes producing a newborn who is quite pissed off to be so violently thrust into this new world.
I think, therefore, that we need to be vary of our use of technology, especially in surgical births. Having a robot do your c-section might sound cool to Bill Gates, until it's you lying on the table, already feeling like a slab of meat and having that inanimate object hovering over you. If you are distressed or emotional about the birth ending in a cesarean, the robot cares even less than your physician might. It doesn't care if you're crying, upset, or having birth trauma. It can't hold your hand throughout or ask how you're doing. It can only, with another machine, check your vitals, see that you're doing okay, and proceed as usual, completely disregarding any emotional or psychological aspects that can't be registered with a machine.
When I had my first cesarean, their routine choice of medication administration was a PCA (patient-controlled anesthesia) pump. This requires an IV be inserted and the patient then decides when to inject herself with pain medication. According to nursing guidelines in the hospital where I gave birth, I was allowed no more than 10 doses in a one-hour period.
This might be all fine and good, and I can understand why a PCA pump can be helpful, if used properly: it allows the patient to determine her level of pain, while the nurse can tend to other patients. But shortly after being wheeled into recovery - probably the minute the spinal wore off - I noticed that I was in increasing pain, and the PCA pump didn't seem to be doing anything about it. Off and on throughout the middle of the night, the pump would routinely beep at me - and I knew, from my experience calibrating pumps as a pharmacy tech - that that meant there was a problem. The nurse would come in every so often, adjust something, tut about this and that, and then leave the room. A half hour or so later, she'd come back for a repeat.
After the first full day, I had tried injecting myself and nothing happened - except a horrible burning sensation up the length of my arm, which had been happening since I was in recovery - and the nurse scolded me that I had reached my maximum number of doses for medication per hour and couldn't have anymore. The pump had counted the number of doses, and it told her I had already had enough, and that was that. No doubt everything else looked good, and she didn't bother asking me why I was still in pain, even with that much medication supposedly flowing through my veins.
Finally, after my hand swelled up like a blown-up latex glove, the nurse noticed and quickly remarked how they 'had to get that thing out of there.' I had told them, numerous times, that it wasn't working, and that I felt more pain from injecting myself than anything else, at this point. I repeatedly asked, "Is it supposed to burn when I do this?" after another dose of Demerol. It was only after that that I realized the line had infiltrated at the injection site and the painkillers were leaching into my tissues, which offered little, if any, pain relief. No explanation, no apology - I only managed to figure out later that that's what happened.
I consider this episode a major technology fail. A machine can give you so many doses of something and then tell the nurse, in a nice digital printout, how much you've had, when you're due for another, and so on and so forth. It cannot, however, tell the nurse why you're in pain, or that there might be a problem. Only she can do that. And she can only do that if she listens to you as a patient.
I had tried speaking up and no one really listened. If they had been listening, perhaps they would have pulled the entire thing out from the beginning and tried again. Another technology fail lies in the fact that, with increased technology, nurses are then able to spend more time tending to other patients, and thus take on a greater caseload. Additionally, when someone does need something that only a human can respond to, they often become resentful or irritated when you do speak up and express a need that the machine failed to address. Perhaps this is why some OB's are perceived - whether for right or wrong - as cold and callous, because they expect the machine to do their jobs, to some extent: to give them results so they don't have to. In many situations, technology - as we see in the case of EFM - has replaced human judgment, which is an art form that is dying quickly, it seems, when it comes to birth. As a result, greater technology has helped patients, while at the same time, hurt them - by destroying the nature of the one-on-one patient-caregiver relationship. No robot can take the place of that.
More reading:
Bill Gates and Robot Cesareans - The Unnecesarean
Wednesday, November 17, 2010
The "C" in ACOG stands for "Castrated"
Posted by
The Deranged Housewife
 OK, call me bitter. But every time I read about a brand new and improved ACOG guideline, especially the latest ones about VBAC and VBA2C being safe, I think, "What's the point? Who is really listening?"
OK, call me bitter. But every time I read about a brand new and improved ACOG guideline, especially the latest ones about VBAC and VBA2C being safe, I think, "What's the point? Who is really listening?"Ever since this summer, the news of the safety of VBAC was on the tip of everyone's tongue and ACOG was urging doctors and hospitals to relax their restrictions on doing them. Yet, thousands of women are still turned away, led to believe no doctor will support them and that they are actually illegal, according to state laws. Thousands more are still telling other women how dangerous they are, even though they know little about them. I'd love to see the figures on what this lack of support is doing to increase the alarmingly high rate of c-sections in the US.
What does ACOG really mean when they restructure guidelines like this, or create new ones? Who's listening? As I decide about having a fourth baby, after two cesareans, what does it mean for me as a patient? And is there any doctor in my county who will "allow" me to have a vaginal birth?
I'm beginning to think that ACOG is the new United Nations, an organization that probably means well but has little power when it comes right down to it. They can shake their fist, demand better, and set 'guidelines,' which is really saying, 'We'd like you to do this, but we are powerless to do anything should you decide to ignore us.' Is ACOG personally going to come after and investigate doctors who have astounding c-section rates? Those who don't do VBACs? Yeah, as if.
One of the biggest reasons for primary cesareans, and in my case as well, is if the baby is breech. I had a primary cesarean in 2003 for breech presentation, and another one last year for breech as well. ACOG's website doesn't necessarily say "we don't recommend a breech birth," but neither do they say "This should be recommended as a way of cutting down on the number of cesareans." Not too many doctors, I suppose, would be willing to admit that a sheer lack of training (among other things, as well) in this area is what leads to a surgical birth. I think that perhaps that would be a blow to your pride, to have to admit that you don't know what the hell to do if a mom comes in at 10 centimeters, waters broken, with a footling breech (been there, done that). So you just whisk them straightaway to the OR.
ACOG's website on this subject actually implies that there are "options" for a mom when she realizes that her baby is breech. Yeah, like "would you like to be sectioned on a Monday or a Tuesday?" While they acknowledge that there can be risks to a vaginal breech birth, they admit that "most breech babies are born healthy." (No where do they mention the skill of a caregiver being able to mitigate significantly risks to you and the baby when he actually knows what he's doing.) Without really coming out and saying it, it's like they're quietly whispering, "If you have your baby vaginally, it'll probably be alright." Not screaming, "YOUR BABY IS GOING TO DIE!" They go on to say that "it's not always possible to plan for cesarean birth," and as your due date approaches, if your baby is breech your doctor "will discuss the risks so that together you can plan the delivery that is best for you." Cue the happy music and the hugely pregnant mom wading through a field of daisies ... I think I am going to barf.
Right! If you read between the lines, ACOG says right there in plain text: "Your doctor will discuss the risks." Of a vaginal birth, you mean. Never a cesarean. This is also what happened to me on at least more than one doctor visit - he sure discussed the risks with me, all right. Let's not mention the benefits of a vaginal birth - like not having a scar on your uterus and all the complications that come with it, both potentially life-threatening and just plain annoying. No more is this underscored than in the death of a mom after her fourth cesarean , due to a combination of placenta problems and doctor error.
This death could have been avoided, some suggest, if more women were encouraged to have VBACs, or - dare we say it - not have a cesarean in the first place, even if the baby was breech.
In this area, I wish ACOG would look north to their Canadian cousins - The SOGC, or Society of Obstetricians and Gynecologists - to get the scoop on how to handle breech vaginal births. It seems, from what they're saying, is you don't have to 'handle' anything: just let it happen, and chances are, the mom and baby will do fine. But that's our biggest problem: they can't keep their hands out of the cookie jar, even when the jar is empty and there's nothing to grab - just leave it alone already and we'll let you know when you're needed.
I'm beginning to think that if ACOG were really serious about lowering the c-section rate and giving women "options," they'd be passing that information on to everyone and her sister and not just allowing it to rest in the often idle hands (and brains) of your well-meaning, but obstinate, physician. Still think your OB is only acting with your best interests at heart?
Monday, November 15, 2010
"He ain't creepy, he's my doula"
Posted by
The Deranged Housewife
I've heard some buzz lately about a new Vince Vaughn movie due (no pun intended) to come out next year called "Male Doula." To some people, this might be the first time they ever hear the word, much less understand what a doula does.
My first exposure to doulas was back when I worked at a newspaper, and the reporter in the cubicle behind me was doing an article on them. I never dreamed I'd ever understand their importance during labor and birth, much less hire one myself one day.
Although our conversation about male doulas on my FaceBook page was meant to be somewhat comical, a reader posted a link about real-life male doula Keith Roberts, who has been serving his clients for over a decade. He rides a Harley, brings a crockpot to warm towels, and helps assist a laboring mother just the way any other doula would, with one exception: he's a man.
This article recounts his time as a massage therapist, and how that segued into becoming a doula. He also tells the rather sad tale of being relegated to watch the births of his two children from behind glass because he, like so many other men in that time period, was barred entry to the delivery room.
There is, apparently, some controversy surrounding male doulas. Some - even members of the Canadian Doula Association, who has no male members - wonder if they are "sickos who get off on childbirth," according to the association's president.
Some find them creepy, and on some message boards I've read, women have said they wouldn't want a man filling that role. Some have even asserted that midwives should be female, too, which I find absurd. If they can offer talents and a level of skill that prevents you from unnecessary interventions and cesarean, and they just happen to be male, are you going to turn them down?
I find that so sad. Yes, there probably are some people who have their weird fetishes, but honestly - would they go to the trouble of getting themselves certified? Why is it that we automatically assume, as our predecessors of the 1960s and 70s, that men who want to support a woman in labor either can't possibly know what they're doing, can't be taken seriously because they don't have a vagina, or are a threat - and are therefore useless in the labor room?
Perhaps Mr. Roberts can provide support to the dad as well, who is often a sounding board for ideas and threats against mom's ability to labor. If there is a supportive male presence in the room to help bolster dad, then he can be a better support system for his laboring partner. When a doctor wants mom to give in to a particular intervention and mom isn't agreeing, they often look to dad in order to strong-arm the patient into consenting. If dad caves in, then mom sometimes follows.
One dad, whose wife had a 40-hour labor with the assistance of Mr. Roberts, said he didn't mind his presence and the couple felt they never would have had the natural birth they desired without Roberts' help. Dad also didn't consider it any different than having a male doctor.
And as it was pointed out, Dr. Biter - who has been nicknamed "Dr. Wonderful" - is very patient-supportive and often called a 'male midwife in disguise.' What's the difference? Dr. Biter, and every male OB out there, have never given birth; but it doesn't mean they can't give you quality care. And really, there are lots of female OBs who probably have never given birth either - so does that really have to be a qualification?
As far as care provider gender preferences, some people prefer a female OB because it's perceived that she is more connected to the pregnant patient by virtue of the fact that she's female, or because she has children, so that makes her a "better" caregiver. However, it's been my experience - and probably lots of other people - that that "connection" somehow gives her the authority to coerce or lead you into certain decisions because "I have a uterus, too, so I know what it's like." Um... not quite.
One man mentioned in the article was apparently barred entry into midwifery and prenatal yoga teaching classes because of his gender, which I find perplexing and sexist. Who's to say he doesn't have anything to offer his clients, even though he's male? I find it sad that our society assumes that there is something somehow wrong or sick with a man wanting to fill a role otherwise reserved for the stereotypically nurturing female. It reminds me of the British dad who was confronted by another female parent because he was photographing his children - and no one else's - while out in public, and she suspected he was a pedophile. Why? Just because he's a male? People often want men to be all warm and fuzzy and "get in touch with their female side!," and yet when they do, they're either perceived as "sickos" or homosexuals. Huh? Just because they're not grunting, standing glassy-eyed in front of the TV, beer can and remote in hand?
As for Mr. Roberts, while he was denied the privilege of supporting his wife Jane in the births of their children, he acted as a doula to his daughters during the births of his two grandchildren. Good for him!
Debbie Young, president of DONA International, thinks that "it takes having a warm heart, a passion for helping pregnant and postpartum women and the training [to make] you a good doula," not whether you're a man or woman, or even if you have personal experience giving birth. I agree!
Regardless of whether the doula is male or female, they've been shown to do tremendous good to the laboring mother. Anyone who can help you manage pain, possibly lower your chances of having a cesarean and just provide attention and support in what can be a somewhat chaotic, sterile environment, is worth it to me, regardless of gender. Who wouldn't want that?
More reading on gender bias and obstetric caregivers:
Burn the Male Midwife! - Rixa Freeze at Stand and Deliver
My first exposure to doulas was back when I worked at a newspaper, and the reporter in the cubicle behind me was doing an article on them. I never dreamed I'd ever understand their importance during labor and birth, much less hire one myself one day.
 |
| Hot towel, anyone? |
This article recounts his time as a massage therapist, and how that segued into becoming a doula. He also tells the rather sad tale of being relegated to watch the births of his two children from behind glass because he, like so many other men in that time period, was barred entry to the delivery room.
There is, apparently, some controversy surrounding male doulas. Some - even members of the Canadian Doula Association, who has no male members - wonder if they are "sickos who get off on childbirth," according to the association's president.
Some find them creepy, and on some message boards I've read, women have said they wouldn't want a man filling that role. Some have even asserted that midwives should be female, too, which I find absurd. If they can offer talents and a level of skill that prevents you from unnecessary interventions and cesarean, and they just happen to be male, are you going to turn them down?
I find that so sad. Yes, there probably are some people who have their weird fetishes, but honestly - would they go to the trouble of getting themselves certified? Why is it that we automatically assume, as our predecessors of the 1960s and 70s, that men who want to support a woman in labor either can't possibly know what they're doing, can't be taken seriously because they don't have a vagina, or are a threat - and are therefore useless in the labor room?
Perhaps Mr. Roberts can provide support to the dad as well, who is often a sounding board for ideas and threats against mom's ability to labor. If there is a supportive male presence in the room to help bolster dad, then he can be a better support system for his laboring partner. When a doctor wants mom to give in to a particular intervention and mom isn't agreeing, they often look to dad in order to strong-arm the patient into consenting. If dad caves in, then mom sometimes follows.
One dad, whose wife had a 40-hour labor with the assistance of Mr. Roberts, said he didn't mind his presence and the couple felt they never would have had the natural birth they desired without Roberts' help. Dad also didn't consider it any different than having a male doctor.
And as it was pointed out, Dr. Biter - who has been nicknamed "Dr. Wonderful" - is very patient-supportive and often called a 'male midwife in disguise.' What's the difference? Dr. Biter, and every male OB out there, have never given birth; but it doesn't mean they can't give you quality care. And really, there are lots of female OBs who probably have never given birth either - so does that really have to be a qualification?
As far as care provider gender preferences, some people prefer a female OB because it's perceived that she is more connected to the pregnant patient by virtue of the fact that she's female, or because she has children, so that makes her a "better" caregiver. However, it's been my experience - and probably lots of other people - that that "connection" somehow gives her the authority to coerce or lead you into certain decisions because "I have a uterus, too, so I know what it's like." Um... not quite.
One man mentioned in the article was apparently barred entry into midwifery and prenatal yoga teaching classes because of his gender, which I find perplexing and sexist. Who's to say he doesn't have anything to offer his clients, even though he's male? I find it sad that our society assumes that there is something somehow wrong or sick with a man wanting to fill a role otherwise reserved for the stereotypically nurturing female. It reminds me of the British dad who was confronted by another female parent because he was photographing his children - and no one else's - while out in public, and she suspected he was a pedophile. Why? Just because he's a male? People often want men to be all warm and fuzzy and "get in touch with their female side!," and yet when they do, they're either perceived as "sickos" or homosexuals. Huh? Just because they're not grunting, standing glassy-eyed in front of the TV, beer can and remote in hand?
As for Mr. Roberts, while he was denied the privilege of supporting his wife Jane in the births of their children, he acted as a doula to his daughters during the births of his two grandchildren. Good for him!
Debbie Young, president of DONA International, thinks that "it takes having a warm heart, a passion for helping pregnant and postpartum women and the training [to make] you a good doula," not whether you're a man or woman, or even if you have personal experience giving birth. I agree!
Regardless of whether the doula is male or female, they've been shown to do tremendous good to the laboring mother. Anyone who can help you manage pain, possibly lower your chances of having a cesarean and just provide attention and support in what can be a somewhat chaotic, sterile environment, is worth it to me, regardless of gender. Who wouldn't want that?
More reading on gender bias and obstetric caregivers:
Burn the Male Midwife! - Rixa Freeze at Stand and Deliver
Sunday, November 7, 2010
Before you get that epidural ...
Posted by
The Deranged Housewife
 |
| In many US hospitals, it's reported that as many as 90 percent of women choose an epidural when giving birth. |
There are two groups: those who were the product of a natural, non-medicated birth, and those whose mothers had epidurals. Their behavior is markedly different, and yet most people think that medicated labors do not produce any effects in the newborn.
I don't know how that's possible. We know that babies can be effected by things in utero that we ingest; even taking Sudafed while nursing, for instance, can produce a jittery baby. There is some debate as to whether the medication crosses the placenta, and I think we can see in this video that there is definitely something going on, to say the least.
I've heard many people say this, including a labor and delivery nurse with supposed years of experience. I'm guessing she hasn't seen many unmedicated births in a while - and she holds the notion that painful childbirth is unnecessary and "why bother?" when you can get pain meds. One mom I talked to said she had an unmedicated birth and that hospital staff were "amazed" at how alert her baby was. No kidding!
In this PregnancyToday question and answer forum, a nurse who teaches childbirth classes asked if epidurals cross the placenta, mainly because a Bradley instructor was telling her clients that they do. The concerned nurse said that it was "her experience" that they didn't. I'm wondering how many natural births she's attended to know what to compare it to - it's a sad reality that many doctors and nurses have never, or very rarely, ever attended a non-medicated birth to know the difference in newborn behavior.
The response (it doesn't say from whom, by the way) immediately slams the Bradley instructor as having an 'extreme' view, and I'm not even sure the answer they gave makes any sense, really:
"As with every extreme position, there is a string of truth. Here are the facts: Local anesthetics cross the placenta. Local anesthetics are used in epidurals. Some local anesthetics placed into the epidural space will be absorbed into the bloodstream and cross the placenta. The small amount of local anesthetic from a properly placed epidural that is absorbed into the bloodstream and crosses the placenta should not affect the mentation of the baby. The lack of affect on the mentation on that baby is an advantage that regional techniques, such as spinals/epidurals, have over intravenous medications."
I'm not sure this really answers the question, and assumes way too much before suggesting that it doesn't ever affect the baby. In one breath, they say the drugs will go into the bloodstream and cross the placenta. Then they turn around and say they should not affect the "mentation" of the baby, but we can see, and some women experience, that it does in fact. Does that mean there are lots of bad anesthesiologists running around, giving bad epidurals? And does this mean they should really admit that the Bradley instructor is right?
I had two cesareans, so obviously I had a spinal for both. In my vaginal birth, I had Nubain but no epidural. I noticed a huge difference in behavior between my babies after birth. Coupled with my inexperience at breastfeeding the first time around, it was difficult to get my oldest to latch on and we spent days - literally - working at it before we were successful. With my second, she took to the breast as soon as I offered it (which, unfortunately due to mother/baby separation that is so typical in American hospitals, was probably at least an hour or two after her birth) and behaved much differently than her brothers did. I don't remember my third being that particularly alert or interested in the breast after birth (again, after being separated from me for several hours).
It could be said that in some babies, the epidural or similar anesthesia can diminish or totally destroy a successful breastfeeding relationship between mom and baby, or at the very least, create a more difficult start to breastfeeding than need be. An inexperienced breastfeeding mom may take this as a sign that baby is totally uninterested in her, and will decide before she even leaves the hospital that breastfeeding is not for her.
It's important to realize that epidurals can be great tools for allowing the mother to relax and labor to progress. But in some cases, they can slow down labor. This is another point of contention among some, but just the other day I heard the amazing birth story of a first-time mother who said that her labor was going pretty fast, and she noticed how the epi slowed it down. For her, this was a good thing because she felt that it allowed her to get her thoughts together. For others, it can be a nightmare that leads to more (and more) interventions, that can sometimes lead to a cesarean - or at the very least, a rather traumatic, difficult vaginal birth.
Studies have shown that epidural use can increase the need for tools such as vacuum suction and forceps - mostly no doubt because some women can't feel what's going on, nor can they get up and change positions when an epidural is in place. Many talk about "light epidurals" (even an anesthesiologist told me about these) but still lots of women say they were completely unable to move due to having one. Again, the jury is out as to whether this is really widespread and may depend on a number of factors, including mother's position and doctor/anesthesiologist preference.
Lastly, we must look at the standard procedure for birth in many hospitals: the mother is likely allowed no food or drink in labor, is encouraged to lie down frequently for cervix checks, is hooked up to a monitor for continuous fetal monitoring, and as a result, is not allowed to move around or really change positions. When it comes to pushing, she is often told she must assume the lithotomy position (flat on her back). When you add all that up, it's not a wonder so many women ask for epidurals and it's amazing a woman can even birth a baby at all.
Remaining upright in early labor can actually make the first stage of labor go faster, and being mobile during labor can help mothers cope with the pain better. Being flat on your back , confined to bed, does not.
It's important to realize that studies have been done, some of which produce completely counterintuitive results. Like, it would seem perfectly plausible that epidurals - especially ones that are "heavy" and allow the mother no sensation whatsoever - would slow down labor. Studies have shown, apparently, that this is not the case. But it's not just as simple as that: it's a multi-faceted issue with lots of pieces to the puzzle that need to be put together before you can draw any conclusion. Since many hospitals and doctors have little idea what normal birth is like, we base the results of many studies - and thus our conclusions about birth - on a completely skewed model of care. Therefore it's important to remember that some studies, however official-sounding, are inaccurate and inherently flawed, especially if they do not take into account those differences.
As I wrote about in this old post , if you choose to get an epidural, that's your decision. It should not be one that's taken lightly, but rather with as much information as possible, so that you have made an informed decision, not one that's based on someone else's perception of pain.
Do epidurals cross the placenta?
Facts on Epidural Anesthesia
Friday, November 5, 2010
Pecking Order
Posted by
The Deranged Housewife
 Did you know that chickens will see a spot of blood or 'defect' on another chicken and eventually peck it death?
Did you know that chickens will see a spot of blood or 'defect' on another chicken and eventually peck it death?This common behavior in the animal kingdom reminds me of how we often behave as humans. It also reminds me of the current fervor over homosexual teens who have, sadly, committed suicide.
I've been seeing links on FaceBook to an excellent blog post by Nerdy Apple Bottom about how her young son wanted to dress up as Daphne from Scooby Doo for Halloween. The post has apparently gone viral, with thousands of comments and page views. It features an adorable picture of her young son in full Daphne regalia, topped off with an enormous flaming orange wig.
As you can imagine, there were some raised eyebrows when the blogger brought her son to his school. Among the reactions were those of some fellow moms, many of whom took it upon themselves to discuss the boy's Halloween costume and what was so "wrong" with it. These bullies were, as the blogger noted, not only bullying her, but her son. And when Mama Bear feels that her cub is being threatened, all hell breaks lose, as it should!
One thing that got me, though: the title of the post is "My son is gay." I realize it was probably her entire point, but really, just because he wants to dress as Daphne doesn't make him gay. Perhaps her point was just that - to address these mothers who thought it was their business to not only point out the obvious, but get up her a@@ about it. I once dated a guy who, according to his elderly grandmother, liked to put on her beads and necklaces and wear them all over the house. He is, as far as I know, a successful attorney who is married and has two daughters. Maybe he passed his beads down to them?
My main issue with the title is even putting it in that context when referring to a little boy, someone who should be more concerned about ... what he wants to be for Halloween, rather than his sexual orientation. Unfortunately, that's hard to focus on when you have adults who want to put you in that category and label you at a time when sexuality shouldn't even be an issue; when it is something, really, that no kid that age should know about or really understand. It's not that he's gay: that's just HIM. It reminds me of a friend I had in college - he wasn't "out" to anyone (yet) and I had a feeling he was gay, but it didn't matter. He was just Andy - not gay or straight.
This blog post really isn't about the sometimes skewed perceptions we have about gender roles. Even though I do think we are hardwired: an acquaintance once tried to hand his son the Barbie doll and his daughter the fire truck in an experiment to get them to play gender-neutrally (or whatever you want to call it), and they promptly rejected the toys and traded. So much for nurture over nature.
What it all boils down to is that in some way, we are all bullies. I find it rather nauseating that suddenly the unfortunate rash of gay teen suicides is being latched on to by the media, the gay community and everyone else at large as a "gay" thing. It's a thing - a thing that effects everyone, on some level - and has nothing, really, to do with gender preference.
I see it all the time among different groups of people with different thoughts and opinions (and everyone's got 'em). Take this election season - the last few elections have not been without drama and a fever-pitch of opinions about certain issues. Whether we're gay or straight; atheist or Christian; right-wing or left-wing - in some ways, we're all bullies. We all have a tendency to latch on to one idea and pick on others who don't share our views, for right or wrong. And many of these people are the same ones who think the current crisis among gay teens is incredibly tragic and "must end now! We must put a stop to bullying!", not realizing they are often just as guilty of the very thing they think is so despicable.
In the mothering community, we see this all the time but probably haven't fully recognized that it's bullying, plain and simple. If we are exclusive breastfeeders, we tend to assume that women who feed their babies formula are only doing so because of X reason. Some even go so far as to call it "poison" - I've seen this many, many times. Or the fervency of people who believe circumcision is wrong and attack those who have their boys circumcised. Or the stay-at-home moms vs. the working moms. And the list goes on...and on ... and on...
Either way, forcing someone to take your point of view, and calling them names like "hater" if they don't, is not espousing tolerance of anyone's diverse opinion except your own. Hello ... that's being a bully. Rather than use the word "tolerance," which is such a token catch phrase that nowadays has little, if any, meaning, perhaps we should use the word "respect" - which carries much more weight and significance.
Unfortunately, it's human nature for us to henpeck each other and to establish a definite pecking order among other people. You can't escape it or try and label it as something else. It's just something we all do - just like chickens, who have brains the size of a small coin. And we think we're so smart.